On the pathogenesis of diabetic retinopathy, damage to muller cells, diseases of opponents, and inflammation: a review
Abstract
Purpose: The purpose of this article is to summarize the literature data of our thirty years research on the pathogenesis of diabetic retinopathy.
Methods: literature data of our and foreign studies.
Results and Conclusion:
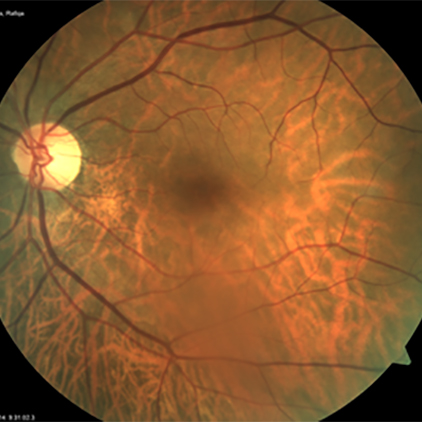
Diabetic retinopathy is a chronic inflammatory process in the retina. It is known that all inflammatory processes occur in the glia. In the retina, one types of the glial cell are Müller cells. There are located between neurons and capillaries. It is their destruction that leads to increased vascular permeability and loss of pericytes.
Lipid peroxidation can damage Müller cells.
There is high activity of glutathione peroxidase in the vitreous body, which neutralize lipid peroxidation. Therefore, these enzymes help the retina neutralize toxic products. An absence of direct contact between the vitreous and the retina’s antioxidant system will severely impair the protection of that part of retina against the harmful effects of lipid peroxidation lipoxidation, which in turn, will accelerate the disruption of cell membranes in retinal neuronal and glial elements, the loss of pericytes, and endothelial damage. Connective tissue can develop at the site of local vitreous detachment. Thus, in diabetic retinopathy, glial cells of the retina are primarily affected.
In diabetes, only the inner part of the retina is damaged, and photoreceptors remain intact. Thus, the inner and outer parts of the retina are opponents. We believe that the positive effect of panretinal laser photocoagulation on diabetic retinopathy is associated with the destruction of the photoreceptor (outer) layer of the retina. That is, artificial retinal dystrophy is induced. In addition, the centre of the retina and its periphery also have an opposing relationship.
Diabetic retinopathy also develops less often in diabetic encephalopathy, dementia. A "parquet type" fundus indicates a lack of blood supply to the vessels of the brain and a risk of ischaemic stroke.
The question is which microbiota is responsible for diabetic retinopathy and other acquired retinal diseases. This is an interesting question that we will answer.